Pregnancy
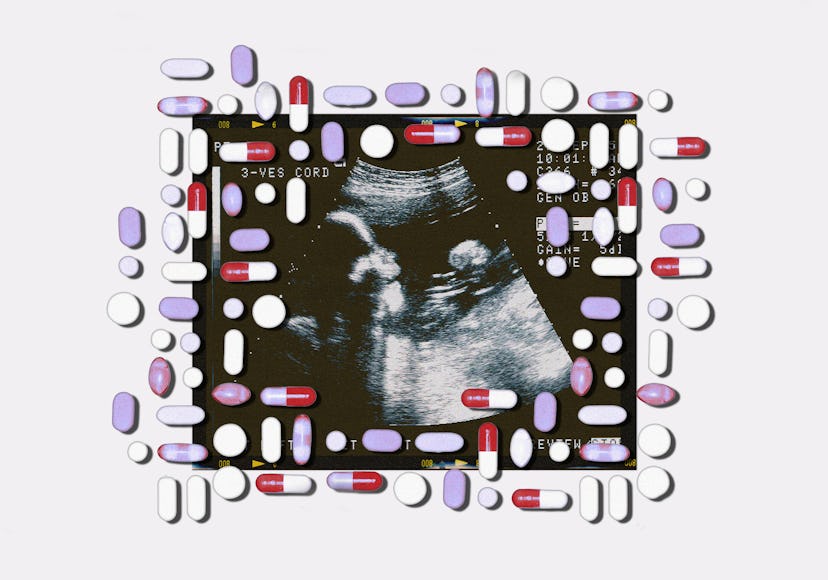
Inside The Uncertainty Of Taking Stimulants While Pregnant
Increasing numbers of pregnant people are resuming their ADHD meds after the first trimester, under the careful guidance of their doctor.
Elizabeth*, 32, has been taking stimulants since the third grade. During her first pregnancy in 2020, her doctor told her she had to stop taking her medication, and she struggled, but felt she had no other choice. “I told myself and my husband in order to be the best mom that I can be while pregnant, I have to do this. I have to do this for myself. I have to do this for my son.”
But by the time Elizabeth was pregnant a second time, the prospect of caring for a toddler without stimulants was daunting, and she had seen other moms on Reddit post about continuing their stimulants through pregnancy. Every time someone posted an update with a photo of their apparently healthy baby, Elizabeth was encouraged.
Elizabeth had been following what little research there was — limited, due to the obvious ethical concerns about doing double-blind studies on pregnant women — but what she did find was reassuring. A 2023 study in Nature found no increased risk of long-term adverse effects on children exposed to ADHD medication in utero, and a systematic review of existing research done in 2020 suggests use of ADHD medication during pregnancy doesn’t result in significant adverse consequences for mother or offspring (though the data is too limited to make an unequivocal recommendation). That’s not to say the medication is without risk: one study found that Adderall use was sometimes associated with an increased risk of low birth weight, poor growth, and preterm delivery.
Elizabeth weighed the risks — low birth weight and preterm labor — and the benefits — feeling like a functional, capable person — and approached her psychiatrist, who approved her decision to start taking stimulants again after 12 weeks of gestation. “It just helped me feel like myself,” she said. Elizabeth was scheduled for extra growth scans because of the risk of low birth weight and though the extra scans worried her, her daughter was born at a completely normal 8 pounds and 11 ounces.
Though Elizabeth was secure in her decision, she mostly kept it to herself, only telling her husband and her closest friends. “I would never tell anybody,” she said. “It’s still such a shameful thing for me to think about sharing.” The use of ADHD medication like Ritalin and Adderall has increased significantly among pregnant women in the U.S., according to the Center for Disease Control and Prevention (CDC), with pregnant people choosing to continue their medication – myself included.
It was my first taste of something I would soon become more and more familiar with: mom guilt.
When I asked Shannon Clark, MD, a professor and maternal-fetal medicine doctor, what she thought was behind this trend, first, she pointed to better diagnostic tools to help diagnose adult-onset ADD/ADHD. Also, she considers the fact that the conversation around medication use during pregnancy was changing rapidly to be a huge contributor to the sea change. “People are starting to ask more questions: What do we know about this medication? What do we not know? What is the risk-benefit? Patients are starting to advocate more for themselves in this conversation, rather than just accepting a blanket ‘stop everything because you’re pregnant’.”
I knew what she meant. I started taking stimulants after a traumatic brain injury, and on the days I didn’t take it, I felt like a slow, blurry shadow version of myself. When I first found out I was pregnant, I was so excited that I cried telling my husband and our families. Underneath my joy, though, was a worry: How would I make it through 40 weeks of pregnancy without the 40 mg of Ritalan I took daily, and had been using to function for years?
But I hated myself a little for even thinking about how I would live without my medication rather than the well-being of this tiny possibility of life, then the size of a poppy seed. That leap from fear to self-reproach, it was my first taste of something I would soon become more and more familiar with: mom guilt.
Because of a mental health history that includes depression and anxiety, I was referred to a perinatal psychiatrist at the UCLA Maternal Outpatient Mental health services (MOMS) Clinic. That doctor would be my saving grace. In our first session, I told the doctor how worried I was about functioning without Ritalin, and the wild spike in anxiety I was experiencing in pregnancy. I told her about my fear that, because of my mental health struggles, my body would be an inhospitable place for my baby to grow.
That’s when my doctor and I came up with a plan: I would abstain from stimulant use entirely during the first trimester, which is widely recognized as the most critical period of development for a fetus. After I passed 12 weeks, I would be able to take Ritalin a few days a week. Then I left my appointment, sat down, and picked at my nails until they bled.
On one hand, I was relieved: I could take Ritalin and it would likely be safe for my baby. On the other, there was the guilt again. My doctors (and my husband and sisters) reminded me that poor maternal mental health also carries a risk of adverse effects, and I knew they were right. Still, I worried that choosing to take the Ritalin meant I had failed the first test of motherhood.
“What pregnant individual is not judged?” Clark asks me. “Everybody has something to say about somebody’s uterus and what’s in it.”
The reasons for Elizabeth’s shame — and mine — are multitudinous. Part of the stigma stems from outdated and downright false ideas about attention-deficit disorders: that they only occur in kids, or can only happen to boys and men, or that the lack of focus is a failure of will. There’s often not a belief in ADHD as a serious or debilitating syndrome and when it is discussed, there’s a focus on how it impacts a person’s ability to work rather than their ability to function in daily life. “I think the world sees it as, you’re just lazy,” Elizabeth said.
“What pregnant individual is not judged?” Clark asks me. “Everybody has something to say about somebody’s uterus and what’s in it.” She emphasizes that further studies are needed, but in general, the calculation of risk to the fetus and the risk to the mother has shifted more generally since she first started training to be an OBGYN, and for the better. “How anyone could think that the fetus comes before the pregnant individual, it defies logic to me,” Clark said. “Because they're making the fetus, right? So you can't neglect the health of the pregnant individual. That's by default, neglecting the health of the fetus.”
Clark clarified to me that even my own decision to continue taking Ritalin was made, in the end, because of my worry that an increase in depression and anxiety would result from skipping my meds would negatively impact my baby. And even though my perinatal psychiatrist assured me that being a mentally healthy mother was the best thing I could do for the health of my baby, I second-guessed the decision, wishing I could cope without it, and feeling shame that I couldn’t.
The topic of stimulant use during pregnancy is a perfect storm: an already misunderstood condition, a lack of studies, and the rush to judgment we have about the decisions pregnant women make. Some of that judgment is internalized, like the dizzying mix of responsibility, guilt, and shame that I’ve found to be threaded through my experience of pregnancy and motherhood so far. But it doesn’t have to be this way. It’s already changing and I hope that as more pregnant people choose to continue stimulants after careful conversations with their healthcare providers and more studies are done, it won’t be as taboo to consider continuing medication.
In the end, I delivered a completely healthy, average-sized baby girl at 40 weeks. Now that I’m on the other side of my pregnancy, I have no doubt that being able to take Ritalin and feel like a semi-functioning person (I suffered from hyperemesis gravidarum, which left me losing weight and throwing up my entire pregnancy) made me a healthier mother. In choosing to prioritize my health and wellbeing, I hope I made my daughter healthier, too.
Fortesa Latifi is a journalist who is currently working on a book about family vloggers and child influencers. She has bylines in places like The Washington Post, The New York Times, and Teen Vogue, among others. You can find her anywhere @hifortesa.